2022: The Year of Automation
Automation is not new to healthcare revenue cycle. For several years now companies have began introducing automation into healthcare. Typically, the slow adoption rate has been caused by limited IT resources and what was sometime considered lower ROI. “The juice wasn’t worth the squeeze” when considering the IT time required to adapt the automation when so many other areas demanded IT bandwidth. That all changes in 2022.
So, what causes the change? Necessity. Most healthcare systems are facing personnel shortages throughout. The revenue cycle is no exception and let’s face it, revenue keeps the lights on. With so many sectors of the economy starving for employees, the trend of increased wages that began in 2021 will continue. Hospitals will be forced to consider anything that can be automated. So, what can you expect to see in 2022 to allow that automation?
Process mining will increase exponentially in 2022 as many healthcare systems move towards Hyper-automation, a holistic approach to automating every aspect possible. Process mining is a review to determine where efficiencies can be gained using technology. Many revenue cycle executives are looking closely at their processes. “We’ve always done it that way” is the most expensive statement is business. Revenue cycle leaders are identifying the areas that can be automated or eliminated as a whole. In many cases, entire processes can be automated and team members can be allocated to other areas where help is needed. Outside vendor partners are available and eager to assist with your assessment for gained efficiency.
Patient Portals and Kiosks have become common in healthcare but many don’t effectively address the financial aspect of a patient’s journey. Look for increasing improvements in these areas. Shifting some of the legacy services to the clients, especially in the Patient Access area will help to alleviate some of the staffing shortages in this area. Additionally, Revenue cycle leaders are looking to provide the patient with more options when it comes to completing their financial obligation. Providing patients one place to view all of their accounts, see their current and historic statements, get help though LIVE chat, set up their own payment plans complete with reminders and make a payment in one place rapidly increases collections in the self-pay area. Patient satisfaction is much higher for those who are unable to take care of their business during the hospital’s normal business office hours and the number of team members needed for customer service is greatly decreased.
RPA Plus is the combination of RPA (Robotic Process Automation; also known as “Bots/Botting”) and AI (Artificial Intelligence). RPA has long been utilized to automate repetitive processes where information was structured and consistent. AI was once known as “Machine Learning” but today is so much more. Automation has historically encountered problems when data was non-structured or needed human interaction. Today, AI includes an intuitive aspect and the ability to understand and adapt. Once trained to capture and interpret actions of specific processes, RPA can then manipulate data, trigger responses, initiate new actions and communicate with other systems autonomously. By combining both RPA and AI, almost any business case can be addressed.
Work Queue Automation follows closely behind RPA Plus as a way to increase efficiencies. By ingesting information, sometimes gathered by RPA Plus but not always, work queue automation can organize and segment that information. Doing so allows workflows to be created that create maximum efficiencies, thus reducing the manhours required to complete the task. A great example is automating insurance claim status. By obtaining the status using a query, the claim response from the payor can be organized into work queues for follow up…or not to follow up. Many hours are spent following up on claims that are already in process/set to pay at the payer. By excluding those claims set to be paid, personnel can follow up on the claims needing attention. Claims to be worked can be segmented into work queues by payer, balance, denial code and many other factors. Denial codes can be interpreted using both CARC and RARC responses to maximize productivity when better understanding the deficiency and what is needed to work the claim.
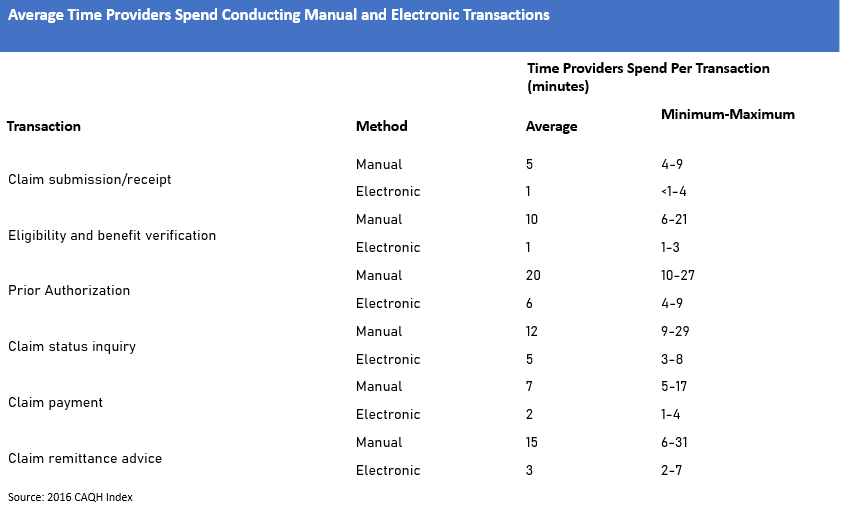
A recent survey by CAQH estimated millions of hours could be eliminated by automating processes in the area of insurance. The average disparity between manual and electronic transactions are shown below. By adding RPA Plus and work queues, the times shown can potentially be decreased even further.
In the current healthcare and employment environment, there has never been a time when automation is more necessary. Successful revenue cycle leaders will mine their processes and partner with companies who are familiar with healthcare revenue cycle and its needs. MedCo provides revenue cycle consulting as well as automation and productivity tools to increase your efficiencies. Call 844-528-4338 today to set up a time to discuss how MedCo can help you reach Revenue Cycle Excellence!
